–°–∫–∞—á–∞—Ç—å —Å —é—Ç—É–± Transplant Rejection, Hyperacute Acute Chronic Graft versus Host –≤ —Ö–æ—Ä–æ—à–µ–º –∫–∞—á–µ—Å—Ç–≤–µ
–°–∫–∞—á–∞—Ç—å –±–µ—Å–ø–ª–∞—Ç–Ω–æ Transplant Rejection, Hyperacute Acute Chronic Graft versus Host –≤ –∫–∞—á–µ—Å—Ç–≤–µ 4–∫ (2–∫ / 1080p)
–£ –Ω–∞—Å –≤—ã –º–æ–∂–µ—Ç–µ –ø–æ—Å–º–æ—Ç—Ä–µ—Ç—å –±–µ—Å–ø–ª–∞—Ç–Ω–æ Transplant Rejection, Hyperacute Acute Chronic Graft versus Host –∏–ª–∏ —Å–∫–∞—á–∞—Ç—å –≤ –º–∞–∫—Å–∏–º–∞–ª—å–Ω–æ–º –¥–æ—Å—Ç—É–ø–Ω–æ–º –∫–∞—á–µ—Å—Ç–≤–µ, –∫–æ—Ç–æ—Ä–æ–µ –±—ã–ª–æ –∑–∞–≥—Ä—É–∂–µ–Ω–æ –Ω–∞ —é—Ç—É–±. –î–ª—è —Å–∫–∞—á–∏–≤–∞–Ω–∏—è –≤—ã–±–µ—Ä–∏—Ç–µ –≤–∞—Ä–∏–∞–Ω—Ç –∏–∑ —Ñ–æ—Ä–º—ã –Ω–∏–∂–µ:
–ó–∞–≥—Ä—É–∑–∏—Ç—å –º—É–∑—ã–∫—É / —Ä–∏–Ω–≥—Ç–æ–Ω Transplant Rejection, Hyperacute Acute Chronic Graft versus Host –≤ —Ñ–æ—Ä–º–∞—Ç–µ MP3:
–ï—Å–ª–∏ –∫–Ω–æ–ø–∫–∏ —Å–∫–∞—á–∏–≤–∞–Ω–∏—è –Ω–µ
–∑–∞–≥—Ä—É–∑–∏–ª–∏—Å—å
–ù–ê–ñ–ú–ò–¢–ï –ó–î–ï–°–¨ –∏–ª–∏ –æ–±–Ω–æ–≤–∏—Ç–µ —Å—Ç—Ä–∞–Ω–∏—Ü—É
–ï—Å–ª–∏ –≤–æ–∑–Ω–∏–∫–∞—é—Ç –ø—Ä–æ–±–ª–µ–º—ã —Å–æ —Å–∫–∞—á–∏–≤–∞–Ω–∏–µ–º, –ø–æ–∂–∞–ª—É–π—Å—Ç–∞ –Ω–∞–ø–∏—à–∏—Ç–µ –≤ –ø–æ–¥–¥–µ—Ä–∂–∫—É –ø–æ –∞–¥—Ä–µ—Å—É –≤–Ω–∏–∑—É
—Å—Ç—Ä–∞–Ω–∏—Ü—ã.
–°–ø–∞—Å–∏–±–æ –∑–∞ –∏—Å–ø–æ–ª—å–∑–æ–≤–∞–Ω–∏–µ —Å–µ—Ä–≤–∏—Å–∞ savevideohd.ru
Transplant Rejection, Hyperacute Acute Chronic Graft versus Host
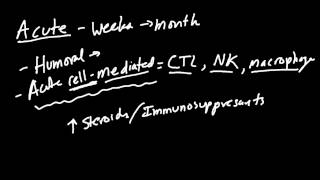
http://www.stomponstep1.com/transplan... SKIP AHEAD: 0:29 – Definition and Introduction to Organ Transplantation 1:50 – Intro to Transplant Rejection 5:00 – The high yield table 6:38 – Hyperacute Rejection 8:22 – Acute Rejection 9:03 – Chronic Rejection 10:34 – Graft vs. Host Disease Organ Transplantation is the replacement of dysfunctional tissue with healthy tissue from “somewhere” else. An individual can receive an organ donation from an animal (such as a pig heart valve) or “donate” tissue to themselves by moving healthy tissue from one part of their body to another (such as skin grafting). However, almost all Step 1 questions are about transplantation from one human to another individual who is not a twin. This type of transplant is known as an Allograft. The donor may be living or recently deceased. A wide variety of tissues can be transplanted, but our discussion will focus primarily on functional organs that require vascular connections like the heart, kidney and liver (not structural tissue like tendons). Blood transfusion is a type of transplant that will be covered in more depth in the Hematology section. When the organ donor is not the recipient themselves or a genetically identical twin, the immune response to the new organ becomes extremely important to prognosis. The grafted tissue expresses antigens that are not present in the host and these antigens are recognized as foreign. The immune system reacts as if the donated tissue is an infectious microbe and attacks the graft. The immune system needs to be kept in check to allow the organ to be moved successfully into the recipient. Transplant Rejection is when there is not immunologic tolerance to the new organ and the host’s immune system damages the transplanted tissue. The damage is often most evident in the vessels of the donated tissue where antigens lining the endothelium come into contact with the immune cells circulating in the hosts blood. Following organ transplantation, patients need to be monitored closely for the onset of symptoms related to dysfunction of the transplanted tissue and they will undergo periodic laboratory evaluation in hopes of identifying rejection as quickly as possible. When rejection is suspected a biopsy is usually done to confirm the diagnosis and rule out another disease process. Hyperacute Transplant Rejection occurs almost immediately and is often evident while you are still in surgery. It is caused by accidental ABO Blood type mismatching of the donor and recipient which almost never happens anymore. This means the host has preformed antibodies against the donated tissue. For example, a recipient with Type B blood would have pre-made antibodies targeted at the carbohydrates on the blood of a Type A donor. The presence of preformed antibodies is why the reaction takes places so quickly. This is an example of Type II Hypersensitivity and results in thrombosis and occlusion of the graft vessel. The transplanted organ must be removed immediately. Acute Transplant Rejection is the most common type of rejection and usually has an onset between weeks and months of the transplant. It is a T-Cell mediated response against foreign Major Histocompatibility Complex in the donated organ. Therefore, it is an example of Type IV hypersensitivity. This process results in leukocyte infiltration of the graft vessel. The risk of Acute Rejection can be diminished (but not eliminated) with prophylactic immunosuppression. If identified early Acute Rejection may be able to be treated with immunosuppressants and corticosteroids. Chronic Transplant Rejection occurs months to years after the transplant. The exact mechanism is not very well understood but it probably involves a combination of Type III and Type IV hypersensitivity directed against the foreign MHC molecules which look like self-MHC presenting a foreign antigen. It results in intimal thickening and fibrosis of graft vessels as well as organ atrophy. Chronic rejection is a slow progressive decline in organ dysfunction while acute rejection is a more rapid decline in function. Chronic Transplant Rejection can be thought of as accelerated aging. There is no treatment available and these patients need to receive a new organ transplant. When Chronic Rejection is suspected a full work up is done to rule out “late onset” Acute Rejection which can be treated. The text for this video is too long for Youtube and exceeds the maximum allowed video description length. To read the rest of it please click here http://www.stomponstep1.com/transplan...